Eye Care Procedures
Cataract Surgery
- State of art phacoemulsification surgery
- Stitchless, no injection topical anaesthesia (drops) technique
- Usually 5 to 10 minutes of surgical time
- Microincision (less than 2mm) surgery
- Torsional Phacoemulsification for better results
- Premium Intraocular Lens implantation
- The State of Art, Optical and Immersion Biometry for accurate IOL Measurement
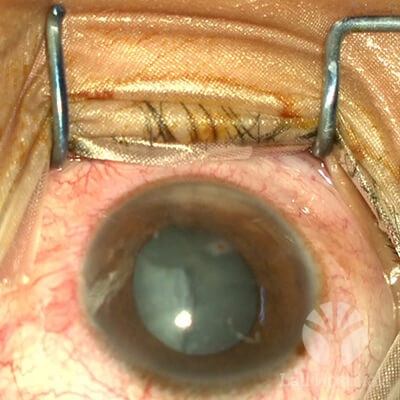
A cataract is a clouding of the clear lens in the eye caused by ageing. As we get older, clumps of protein may form and begin to cloud the lens, reducing the light that reaches the retina. Cataract surgery is a procedure to surgically remove the cloudy lens of the eye and, in most cases, replace it with a clear, artificial lens.
Causes
Ageing, eye injuries, other eye conditions or surgery, medical problems such as diabetes, and hereditary disorders are probable causes of cataract.
Symptoms
Patients notice a gradual blurring or dimming of vision or decreased colour perception. Some people see a halo or haze around lights, especially at night, or experience double or multiple vision. At first, the symptoms may only occur in dim light or when the patient faces bright oncoming car headlights, making night driving especially difficult.

Treatment
Cataract surgery is one of the safest and most effective procedures performed today. Cataract removal is typically done as an outpatient procedure, with quick recovery time.
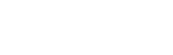
- Phacoemulsification – During phacoemulsification, the most common treatment for cataract surgery, a tiny incision is made in the front of the eye (cornea). A needle-thin probe is inserted into the lens substance where the cataract has formed. The probe, which emits ultrasound waves, is used to break up (emulsify) the cataract and suction out the fragments. The lens capsule at the very back of the lens is intact to serve as a place for the artificial lens to rest. Also known as a small incision approach, it is generally bloodless, and sutureless, i.e. stitches are usually not used to close the tiny incision in your cornea at the completion of the procedure.
Performed under topical anaesthetic, the procedure only lasts between 5- 15 minutes. We at Lall Hospitals perform this procedure using the latest Alcon Infinity Phaco Emulsification System, one of the best technological advancements in cataract surgery. It uses Ozil or Torsional Phaco for the best results.
- Extracapsular Cataract Extraction – Occasionally an older cataract surgery technique called extracapsular cataract extraction may be performed in case of specific eye complications. In this procedure, a larger incision is made through which surgical tools are used to remove the lens in one piece, leaving the back part of the capsule intact to allow for implantation of an intraocular lens. After the cataract has been removed, the incision is closed with sutures (stitches).
Intraocular Lens (IOL)
- All kinds of Intraocular Lenses available to suit everyone’s need
- Premium Monofocal Aspheric, Blue Light filtering, Preloaded Lenses for crisp and clear vision
- Toric Intraocular lenses for Cylindrical Powers i.e. Astigmatism
- Multifocal Lenses for distance and near correction
- Trifocal lenses for distance, intermediate and near correction
- Extended Focal length intraocular lenses
- Correction of aphakia by Retro-fixated IOL
An IOL is a permanent replacement for your natural lens. Today, doctors try and bring patients as close to perfect vision as possible, without the use of glasses, through the use of IOLs. Made of plastic, acrylic or silicone, IOLs are implanted in the empty capsule of your eye during cataract surgery. The IOL requires no care and becomes a permanent part of your eye.
Types of IOL
The different types of IOLs available are:
- Monofocal – They designed to correct vision at one focal length, far or near.
- Multifocal – These lenses are similar to glasses with bifocal or progressive lenses. Different areas of the lens have different focusing strengths, allowing for near, medium and far vision.
- Toric Lens – These lenses correct astigmatism, an irregularity in the curvature of the cornea.
- Multifocal Toric Lenses – They are designed to correct for near and far distances and astigmatism.

Laser Vision Correction
- Spectacle removal for Myopia, Hyperopia and astigmatism
- Wave front Guided Lasik for High Definition Vision
- I Design 2 (Customised LASIK) for aberration measurements, providing the precise correction.
- Implantable Collamer Lens (ICL) implantation for patients not suitable for LASIK Corneal Diseases
- Skilled, trained cornea specialist
- Government certified corneal transplant centre with facilities for full-thickness and lamellar corneal transplants (DSAEK & DALK) with excellent outcomes
- Pterygium, corneal infections and ocular surface diseases management including Amniotic membrane grafts with fibrin glue
- Complete keratoconus management including Pentacam, C3R (collagen crosslinking), RGP and Rose K contact lenses fitting
Laser vision correction, also known as refractive surgery, treats near-sightedness, far-sightedness, and astigmatism, helping to eliminate the need for eyeglasses and contact lenses for many patients. An outpatient procedure, it uses a special type of cutting laser to change the shape of the cornea to enable light entering the eye to be properly focused onto the retina for clearer vision.
Refractive Error
Normally, the rays of light entering the eye are brought to a precise focus on the retina – the light-sensitive layer lining the back of the eye. A refractive error results when such a focus is not achieved, with unclear vision. These imperfections in the focusing power of the eye are called refractive errors.
- Myopia or Near-sightedness – A myopic eye is longer than a normal eye or has a cornea that is too steep, as a result of which the light rays focus in front of the retina. Close objects look clear, but distant objects appear blurred.
- Hyperopia or Far-sightedness – This involves an eye that is too short or a cornea that is too flat, as a result of which images focus at a point behind the retina. People with hyperopia can usually see distant objects well but have trouble focusing on nearby objects.
- Astigmatism or Cylindrical Error – This occurs when the incoming light rays are unable to reach a common focus within the eye. Astigmatism distorts or blurs vision for both near and far objects. Having astigmatism in combination with myopia or hyperopia is possible.


Treatment
At Lall Hospitals, we offer two types of treatments for refractive error correction:
- Laser In-Situ Keratomileusis (LASIK) – In this surgical procedure, a thin hinged flap of cornea is created and lifted to one side to access the underlying cornea (called the stroma) and remove some corneal tissue using an excimer laser. The flap is then repositioned in its original position. This technique allows surgeons to reshape the cornea by removing the corneal tissue without disrupting the surface of the eye resulting in restoration of perfect vision.
- Photorefractive keratectomy (PRK) – In this procedure, the thin outer layer of the cornea (epithelium) is removed and discarded prior to reshaping the underlying corneal tissue with an excimer laser. The epithelium repairs itself (grows back over the corneal surface) within a few days after surgery, resulting in a longer recovery time.
Retinal Diseases
- Skilled, fellowship-trained, Retinal Super specialists
- Fundus Fluorescein Angiography, Optical Coherence Tomography, ultrasound for the diagnosis of retinal diseases.
- Intravitreal Injections of Ozurdex, Anti Vegf – accentrix and Antibiotics with vitreous biopsy, if needed
- All types of Retinal Lasers
- Skilled management of endophthalmitis (intraocular infections) and other post-operative complications
- Retinal detachment, macular hole, Advanced Diabetic retinopathy surgeries.
- Retinopathy of Prematurity Diagnosis and management
- Diagnosis and management of optic nerve diseases
- Management of Hypertensive Eye Diseases.
- 23- and 25- Gauge Suture less vitreoretinal surgeries.
The retina is a thin layer of tissue at the back of the eye with light-sensitive cells that gather and process visual information. This is relayed to the brain through the optic nerve which enables us to see. Retinal diseases can affect any part of the retina.
Symptoms
Many retinal diseases share some common signs and symptoms. These may include:
- Seeing floating specks or cobwebs
- Blurred or distorted vision
- Defects in the side vision
- Loss of vision


Types
Retinal diseases vary widely but are mostly related to ageing, trauma and other disorders, threatening the normal functioning of the retina. Some of the most common are:
- Diabetic Retinopathy – Diabetic retinopathy develops as the blood vessels of the retina become damaged over time by elevated blood sugar levels. Read More
- Retinal Detachment – Retinal detachment is often the result of a tear or a hole in the retina, which allows gel-like material from the vitreous of the eye to pass through and collect under the retina. The detachment occurs when the thin layer of tissue that lines the inside of the eye (the retina) is lifted or pulls away from its normal position.
- Macular Hole – A macular hole is a small defect in the centre of the retina at the back of the eye (macula). The hole may develop from abnormal traction between the retina and the vitreous, or it may be the result of an eye injury.
- Macular Pucker – When a thin membrane grows on the surface of the centre of the retina (the macula), it creates a condition known as macular pucker. This abnormality can contract, or pull on the retina, resulting in distorted or blurred vision.
- Age-related Macular Degeneration – This affects the centre of the retina resulting in blurred central vision or a blind spot in the centre of the visual field. Early symptoms include difficulty in adjusting to lower light levels, blurring or distortion, and eventually reduction in vision.
- Cystoid Macular Edema – This condition is characterised by swelling (edema) in the macula as a result of pockets of fluid that accumulate as a result of inflammation or mechanical traction, resulting in blurry or wavy vision.
- Eye Stroke or Retinal Vein Occlusion – A blockage in a small vein that returns blood from the retina to the heart is referred to as a retinal vein occlusion. This obstruction, typically caused by a blood clot, can result in fluid build-up in the surrounding macular tissue severely impacting vision. Eye stroke can cause permanent damage to the retina and vision loss if not treated immediately.
- Retinitis Pigmentosa – This refers to a group of inherited visual disorders which affect the light-sensitive cells in the retina, resulting in a gradual deterioration of vision. This typically affects the peripheral retina early and progresses later to compromise the central vision, resulting in blindness. Early symptoms include progressive night blindness and sudden flashes of light.
- Retinal Inflammatory Disease – It is an eye condition, also known as Uveitis, that causes dysfunction of the retina and, in the most severe cases, substantial vision loss. Read More
Diagnostic Tools
These latest diagnostic imaging solutions can be conducted to determine the location and extent of the retinal disease:
- Spectral-Domain Optical Coherence Tomography (SD OCT) – This rapid, non-invasive imaging technology captures precise images of the retina which is critical in diagnosing retinal diseases and also in monitoring responses to treatment.
- Wide-Field Digital Fundus Photography – A high resolution, wide-field digital fundus camera is employed for examining and evaluating the periphery of the retina. The peripheral retina is the site of many retinal diseases which are difficult to detect with the conventional imaging devices.
- Fluorescein Angiography – This test uses a dye that causes blood vessels in the retina to stand out under a special light, helping to accurately identify closed, leaking or new abnormal blood vessels and subtle changes in the back of the eye.
- Ultrasound – This test uses high-frequency sound waves (ultrasonography) to help view the retina and other structures in the eye to identify certain tissue characteristics that can help in the diagnosis and treatment of eye tumours.


Treatment
The treatments of retinal diseases include:
- Laser Surgery – Laser surgery is used to repair a retinal tear or hole by heating small points on the retina. The resultant scarring usually binds the retina to the underlying tissue. Immediate laser treatment of a new retinal tear can decrease the chances of a retinal detachment.
- Scatter Laser Photocoagulation – This technique is used to shrink abnormal new blood vessels that are bleeding or threatening to bleed into the eye and may help people with diabetic retinopathy.
- Freezing – In this process, also called cryopexy, a freezing probe is applied to the external wall of the eye to treat a retinal tear. Intense cold reaches the inside of the eye and freezes the retina, resulting in a scar that secures the retina to the eye wall.
- Pneumatic Retinopexy – This technique is used to help repair certain types of retinal detachment and can be used in combination with cryopexy and laser photocoagulation.
- Scleral Buckling – A small piece of silicone is sewn to the outside eye surface (sclera), indenting the sclera and relieving some of the force caused by the vitreous tugging on the retina. This technique may be used in conjunction with other treatments.
- Vitrectomy – This procedure involves the removal of the gel-like fluid that fills the inside of the eye (vitreous) and injecting air, gas or liquid into that space. Vitrectomy may be used if bleeding or inflammation clouds the vitreous and may be a part of treatment for people with a retinal tear, diabetic retinopathy, a macular hole, an infection, eye trauma or a retinal detachment.
- Injecting Medication – Medication may be injected in the eye and is effective in treating patients with wet macular degeneration, diabetic retinopathy or broken blood vessels within the eye.

Diabetic Retina Care
- Fundus Fluorescein Angiography and Optical coherence Tomography
- Skilled Fellowship Trained Retina Specialists
- Intravitreal Injections – Ozurdex and Accentrix
- Retinal lasers
- 23- and 25- Gauge Suture less Vitreoretinal Surgery for Advanced Retinopathy
Diabetes puts patients at risk of diabetic retinopathy. Blood vessels in the light-sensitive tissue at the back of the eye, the retina, are damaged over time as a result of increased sugar levels. Diabetic Retinopathy progresses through a series of stages – mild nonproliferative retinopathy, moderate nonproliferative retinopathy, severe nonproliferative retinopathy and proliferative retinopathy.
Symptoms
Symptoms may not appear in the initial stages of the medical condition, but as it progresses, the following symptoms may be noticed:
- Spots or dark strings floating in the vision known as floaters
- Blurred vision
- Fluctuating vision
- Impaired colour vision
- Dark or empty areas in the vision
- Vision loss
Diagnosis
These procedures are used to diagnose, document and follow up on the various levels of diabetic retinopathy.
- Digital Retinal Photography and Digital Fluorescein Angiography – These procedures begin with eye drops being put into the patient’s eyes to dilate them, enabling a better view inside the eyes. A yellow dye, called fluorescein is then injected into a vein on the patient’s arm. The dye travels through the blood vessels while a special camera takes photos of the retina as the dye moves throughout. Any blood vessels that are blocked, leaking fluid or show an abnormal growth are immediately tracked.
- Optical Coherence Tomography – This imaging test provides cross-sectional images of the retina that show the thickness of the retina, which helps determine whether fluid has leaked into the retinal tissue and further, to monitor the treatment.

Treatment
At Lall Hospitals, we offer the following procedures for patients of diabetic retina care depending on their stage of diabetic retinopathy:
- Eye Injections – Anti-VEGF (Vascular Endothelial Growth Factor) is the first line of treatment in which the medicine is directly injected into the eye to block the growth of abnormal blood vessels and reduce swelling. Administered under local anaesthesia, the treatment requires injections at regular intervals depending on the severity of the condition.
- Retinal Laser Photocoagulation – This laser treatment, also known as focal laser treatment, can stop or slow the leakage of blood and fluid in the eye. Faster and more comfortable than standard laser procedures, leaks from abnormal blood vessels are treated with laser burns.
- Surgery – Vitrectomy is a surgical procedure where the vitreous, the clear, gel-like substance in the central chamber of the eye is removed, enabling removal of blood that may have leaked into it and clouded vision or of scar tissue that may be pulling on the retina, producing a detachment. Laser treatment is often performed as part of the procedure, and the cloudy vitreous is replaced with a clear saline fluid, replaced over time by the eye’s own replacement liquid.
Squint
- All kinds of Cosmetic and Functional Squint treatment
- Amblyopia (lazy eye) therapy
- Skilled squint specialist
- Prismatic lenses
A squint or strabismus is a medical condition in which the eyes do not look in the same direction, at the same time and hence are not correctly aligned. This misalignment may be constant, being present throughout the day or may appear sometimes. A squint can affect babies, children or adults and must be treated immediately for better results.
Causes
The major causes of having a squint are poor eye muscle control, an improper balance of eye muscles, faulty nerve signals to the eye muscles due to a nerve injury or illness, long sight which develops as the eyes over-focus in order to see clearly and congenital squint, a family history of squint.
Symptoms
Symptoms may be difficult to detect as an unusual looking eye can be mistaken for a squint. However, blurred vision and lazy eye (amblyopia), in which eye muscles do not detect signals from the brain, are common symptoms.


Treatment
Eye tests are conducted to determine the extent and type of strabismus based on which several lines of treatment may be advised.
- Vision Glasses – These should be worn regularly to correct vision problems (refractive errors).
- Eye Exercises – Eye exercises help in restoring eye-coordination.
- Medication – Botulinum toxin injections are given into the eye muscles which allow eyes to realign by weakening the muscles.
- Corrective Surgery – Also known as strabismus surgery, it usually involves the tightening or moving of one or more of the outside eye muscles to help move the eyes and change their position. An outpatient surgery, it is performed under local anaesthesia for adults and general anaesthesia for children.
Oculoplasty
- Treatment of congenital as well as acquired nasolacrimal duct block with Syringing, Probing and Surgery (DCR)
- Lid related diseases like chalazion, stye, blepharitis, entropion, ectropion, Ptosis, lid tumour, lid injuries, congenital lid malformations
- Botox treatment for Blepharospasm, Wrinkles, antiaging
- Ocular and orbital tumours
Oculoplasty is plastic surgery focused on the structures surrounding the eye, including the eyelids, orbit (bones of the eye socket), the lacrimal system (tear duct system), forehead, and the midface area. These surgeries may be performed to correct or treat a medical condition, an injury or for cosmetic purposes.
Some common disorders include:
- Droopy Eyelid
In this medical condition, the eyelids may become droopy or heavy due to excess eyelid skin (dermatochalasis), sagging eyebrows (brow ptosis) or weak eyelid muscles (ptosis). The malposition of the eyelids may affect their appearance or function even causing vision problems.
Depending on the reason for the droopy eyelid, the following treatments may be recommended:
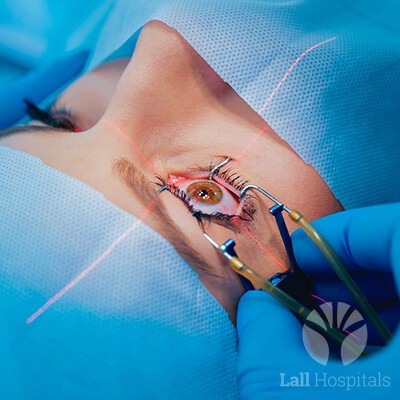
- Blepharoplasty – In cases of dermatochalasis, the excess eyelid skin and fat is surgically removed.
- Ptosis Surgery – The weakened eyelid muscles are re-connected to raise the eyelids.
- Brow Lift – When the reason for the eyelid malposition is sagging eyebrows, a brow lift is advised.
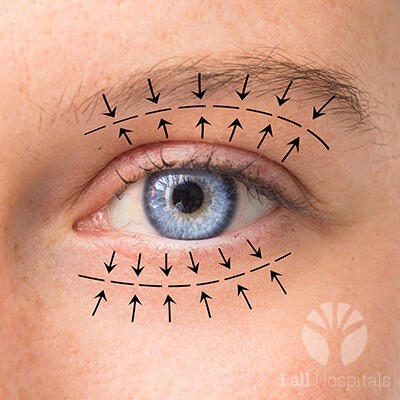
- Tear Duct Obstruction
The lacrimal system in the eye keeps the eye adequately lubricated by producing and draining tears. A nasolacrimal duct (the drain-pipe of the eye) is responsible for draining the tears from the eye. When this duct becomes obstructed, it can cause excessive teas, redness of the eye, and infections.
This obstruction can be corrected through a surgery called dacryocystorhinostomy (DCR) wherein a new tear drain opening, bypassing the blockage in the nasolacrimal duct is created to drain out the tears.
- Eye Lesions and Tumours
Eye lesions are abnormal growths of tissue that can be benign or malignant while tumours can grow in the eye socket or orbit, the space behind and around the eyeball, displacing the eye or pushing it forward to create a bulging effect known as proptosis.
The first step in the treatment is to determine whether the eye lesion is cancerous or not through a biopsy. Further, two lines of treatment can be prescribed:
- Malignant cancers of the eyelid are most often removed through surgery, after which the eyelid’s appearance and function are repaired and restored through highly specialised plastic (reconstructive) surgery.
- Orbital tumours are treated through a combination of surgery, radiation, and chemotherapy.


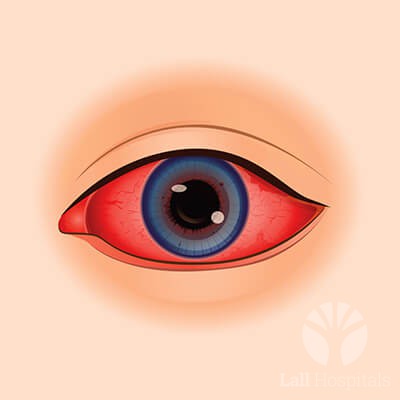
Glaucoma
Glaucoma is used to describe many related conditions that cause damage to the optic nerve which transmits information from the eye to the brain. Though usually associated with high intraocular pressure (high pressure in the eye), sometimes the optic nerve damage can occur even when the intraocular pressure is normal. Without treatment, glaucoma can progress to a permanent, irreversible vision loss.
Symptoms
The only symptom is a gradual loss of vision which is often not noticed. When symptoms are present, they may include:
- Sudden severe eye, eyebrow pain or a headache
- Nausea and vomiting
- Blurred vision
- Halos around lights
- Sudden loss of sight
- Eye redness
Types
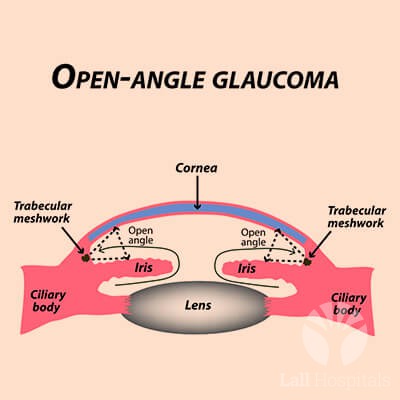
The glaucoma disorder is usually divided into two groups—open-angle glaucoma and angle-closure glaucoma. This distinction is vital in determining the appropriate treatment for the condition.
Open Angle Glaucoma
Open Angle Glaucoma is the most common form of the disorder and can be divided into the following sub-types:
- Primary Open Angle Glaucoma – This form of glaucoma occurs when the eye’s drainage meshwork becomes clogged resulting in a fluid build-up over time which increases the pressure inside the eye.
- Secondary Open Angle Glaucoma – This is the result of other medical or ophthalmic conditions like high blood pressure, poorly controlled diabetes, traumatic eye injury, uveitis, an advanced case of cataracts or drugs like steroids. It may occur in one or both eyes. Secondary forms of open-angle glaucoma include:
- Uveitic Glaucoma – Uveitis causes swelling of the middle layer of the eye. When the inflamed cells block the eye’s drainage canals, preventing fluid outflow, the intraocular pressure in the eye may increase, resulting in uveitic glaucoma.
- Pseudoexfoliation Glaucoma – This type of glaucoma occurs when a flaky material peels off from the outer layer of the lens, obstructing the eye’s drainage system.
- Pigment Dispersion Glaucoma – This is triggered by the shedding of pigment granules from the iris jamming drainage the canals in the eye, leading to a slow pressure build-up.
- Neovascular Glaucoma — New blood vessels form on the iris and over the eye’s drainage channels as a result of uncontrolled diabetes. This abnormality blocks fluids from leaving the eye, causing the intraocular pressure to rise, leading to neovascular glaucoma.
- Low-tension Glaucoma – This occurs when the optic nerve is damaged despite a normal eye pressure. Risk factors include a family history of the disease, a history of systemic heart disease like irregular heart rhythm, and low blood pressure.
- Juvenile Glaucoma – A rare open-angle glaucoma that develops between the ages of 3 and young adulthood, juvenile glaucoma is associated with a variety of genetic defects. Symptoms include myopia (near-sightedness), tearing and light sensitivity.
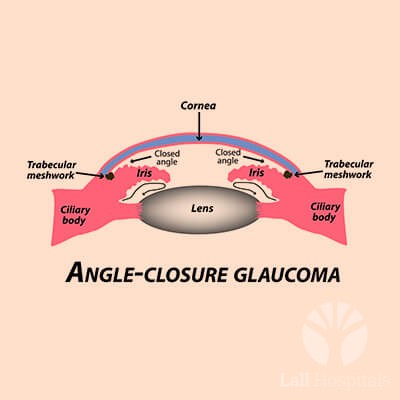
Closed Angle Glaucoma
A less common form of glaucoma, the angle between the iris and cornea in this type of glaucoma is narrowed or blocked causing a sudden increase in intraocular pressure. Also known as narrow-angle glaucoma, its onset can be either abrupt or slowly progressive.
The following are the different sub-types of angle-closure glaucoma:
- Acute Angle-Closure Glaucoma – A medical emergency that can result in vision loss within hours if treatment is not started immediately, acute angle-closure glaucoma occurs from sudden, complete blockage of the drainage meshwork and an abrupt rise in intraocular pressure.
- Chronic Angle-Closure Glaucoma – In this form of glaucoma, the blockage may occur slowly over time as scar tissue forms in areas where the iris is in contact with the drainage channels. As the rise in eye pressure is gradual, the usual symptoms are generally absent, despite marked pressure elevation, causing vision damage.
- Secondary Angle-Closure Glaucoma – This develops as the result of other medical or ophthalmic conditions, like the secondary open-angle glaucoma and can occur in one or both eyes. These may include poorly controlled diabetes, traumatic eye injury, certain drugs, advanced cataracts and uveitis.
Diagnostic Tools for Glaucoma
A wide range of diagnostic tools are used for a detailed clinical examination, including:
- Pentacam – Corneal topography is a computer-assisted diagnostic tool that creates a three-dimensional map of the surface curvature of the cornea. The three-dimensional map is a valuable aid in assisting the diagnosis and treatment of a number of conditions including refractive surgery and keratoconus.
- Pachymeter – An ultrasound device used to measure the thickness of the cornea. Research has shown that central corneal thickness increases the risk of glaucoma in cases of elevated intraocular pressure.
- Tonometer – A quick and painless procedure to determine the fluid pressure inside the eye.
- Visual Field Test – As peripheral vision is usually affected by glaucoma before central vision, this test is conducted to determine the amount of peripheral vision that has been lost in an effort to diagnose glaucoma.
- Gonioscopy – This procedure entails the examination of the trabecular meshwork and the angle of the eye where fluid drains, through a slit lamp, to determine if it is open or closed. A closed or nearly closed angle is a risk factor for angle-closure glaucoma.
- Optical Coherence Tomography (OCT) – This non-invasive imaging test uses light waves to take cross-sectional pictures of the complex biological structures of the eye. These include the thickness of the nerve fibre layer and a three-dimensional representation of the optic nerve, which are helpful in the diagnosis of glaucoma.


Treatment
Early diagnosis and treatment are vital to preserving a patient’s vision. The primary treatment options for glaucoma, include:
Open Angle Glaucoma is the most common form of the disorder and can be divided into the following sub-types:
- Medications for Glaucoma – Most medications for glaucoma are administered in the form of eye drops. Most work either by decreasing the amount of fluid produced by the eye or improving the drainage of eye fluid.
- Surgical Treatment of Glaucoma – Surgery for glaucoma may be recommended when eyedrops fail to reduce eye pressure adequately. Some surgical techniques used to improve the eye’s drainage include:
- Laser Trabeculoplasty – Low-energy laser pulses are applied to the eye’s drainage tissue prompting chemical and biological changes that improve the reduced drainage.
- Trabeculectomy – A procedure in which the eye pressure is lowered by making an opening into the front chamber of the eye, allowing fluid to drain to the surface.
- Glaucoma Drainage Implants – A small silicone tube is placed in the front or back chamber of the eye, bypassing the eye’s damaged outflow system and draining fluid to a reservoir which is positioned on the surface of the eye, beneath the eye’s lining skin.
- Laser Iridotomy – A procedure to treat angle-closure glaucoma using the advanced Nidek Laser, laser iridotomy involves the creation of a tiny hole in the iris (the coloured part of the eye), allowing for the passage of fluid from the back chamber of the eye to the front chamber where it can access the eye’s drainage channels.
Trauma
- 24×7 availability for any emergency ocular trauma
- Skilled super-specialist retina and cornea surgeons
- Corneal and scleral tear, traumatic cataract and infections management
- Eye trauma repairs with state of art vitrectomy and total anterior segment reconstruction
- Metallic as well no metallic Intraocular Foreign Body management
- All kinds of Industrial and other Accidental Eye Trauma Care
- Chemical injuries management with amniotic membrane and limbal stem cell transplant
Eye trauma refers to injury to the eyes and its surrounding areas due to accidents, burns or objects hitting the eye.
Symptoms
Symptoms of eye trauma may include:
- Bruising (black eyes)
- Cuts to the eyelid
- Eye redness
- Swelling
- Bleeding between the cornea and iris, known as hyphema
- Retinal detachment
- Blurred or cloudy vision
- Double vision
Treatment
The treatment prescribed depends on the severity of the trauma and may range from application of a cold press to bring the swelling down to reconstruction of the eyelids and eye socket (the cavity of the skull that holds the eye in place).

Corneal Diseases
The cornea is the eye’s outermost layer. It is the clear, dome-shaped surface that covers the front of the eye and transmits light to the interior of the eye, allowing us to see clearly. It plays a vital role in focusing vision. Injuries and diseases, sometimes hereditary, can cause clouding, distortion or scarring of the corneal tissue. The result, depending on the nature and extent of the problem, may be reduced vision, pain, sensitivity to light, redness, tearing and inflammation.
Inherited Corneal Diseases
- Keratoconus – A non-inflammatory condition, keratoconus occurs when the cornea thins and gradually bulges outward into a cone shape, causing blurred vision or distorted vision, near-sightedness, high irregular astigmatism and increased sensitivity to light.
- Fuchs’ Endothelial Dystrophy – Fuchs’ dystrophy is a condition where the endothelial cells that line the inner surface of the cornea slowly start to die. As more and more cells are lost, fluid begins to build up, causing swelling in the cornea. The disorder can lead to glare, cloudy vision and eye discomfort. Fuchs’ dystrophy usually affects both eyes and can cause your vision to worsen over years gradually.
- Map Dot Fingerprint Dystrophy – Map-dot-fingerprint dystrophy affects the back layer of the epithelium (the cornea’s outermost layer), which separates it from the stroma. It grows irregularly, which causes irregularities in the cornea that look like maps, dots, and small fingerprints.
Diagnostic Tools
- Pentacam – Corneal topography is a computer – assisted diagnostic tool that creates a three-dimensional map of the surface curvature of the cornea. The three-dimensional map is a valuable aid in assisting the diagnosis and treatment of a number of conditions including refractive surgery and keratoconus.
- Optical Biometry – The current standard for intraocular lens (IOL) power calculations in clinical practice, optical biometry is a highly accurate non-invasive automated method for measuring the anatomical characteristics of the eye. Accurate measurements are critical for determining the correct power of an IOL before it is implanted during cataract surgery.
Treatment
- Corneal Collagen Cross Linking – A safe, effective, and relatively simple treatment, this procedure aims to halt the progressive and irregular changes in the corneal shape known as ectasia by stabilising the corneal contour and improving visual function in some patients. The most common form of ectasia is keratoconus. Cross-linking of collagen refers to the ability of collagen fibrils to form strong chemical bonds, i.e. cross-links with adjacent fibrils. The corneal collagen is crosslinked with the help of ultraviolet rays (UVA) and a photosensitiser, Riboflavin, enhancing the rigidity of corneal tissue and stabilising the condition.
Corneal collagen cross-linking is most effective when done in the early stages of the disease before the cornea has become too misshapen and vision has been compromised. At Lall Eye Care Centre, we have the latest machine, the PXL Platinum 330 to perform this procedure. Performed under topical anaesthesia, the treatment is painless and lasts for an hour, at the end of which the eye is patched.
- Laser Vision Correction – This technique allows surgeons to reshape the cornea (with the help of a special flap-cutting laser) by removing corneal tissue without disrupting the surface of the eye. Read More

Uveitis and Ocular Immunology
- All kinds of Ocular Inflammation diagnosis and management
- Latest immunotherapy with disease-modifying treatments, biologicals and immunosuppressive treatments.
- Management of complications with laser or surgery
- Well trained specialists
Uveitis is a form of eye inflammation which affects the middle layer of tissue in the eye, known as the uvea. If left untreated, uveitis can be serious, leading to a permanent loss of vision.
Symptoms
Symptoms include redness of the eye, pain and light sensitivity, blurred or decreased vision. These may develop gradually or may occur suddenly.
Causes
In most cases, it is difficult to ascertain the cause of uveitis. However, the most common causes of uveitis are autoimmune diseases, where your body attacks itself, like rheumatoid arthritis, lupus, and sarcoidosis, trauma to the eye, herpes, shingles, histoplasmosis (a fungus) and toxoplasmosis (a parasite).
Types
The type of uveitis depends on the part of the eye it has affected:
- Anterior Uveitis affects the front of the eye and is the most commonly occurring. It is often called iritis because it mainly affects the area around the eye’s iris.
- Intermediate Uveitis is inflammation of the ciliary body, the front end of the retina, and the vitreous.
- Posterior Uveitis is the inflammation of the choroid, retina and optic nerve.
- Panuveitis occurs when all layers of the uvea are inflamed.
Treatment
The first step of the treatment is steroidal eye drops to reduce the inflammation and pain. The second line of treatment is steroidal injections or oral medication. For recurring cases of uveitis, patients may be prescribed immunosuppressive drugs which subdue the immune system.